Low Back Pain
Low back pain (LBP) is the most common symptom reported by chiropractic patients. It can drastically affect quality of life - both physically, emotionally, and financially.
From 2000-2007, the total number of adults with chronic low back pain has increased by 64%.
One out of every 5 people are experiencing low back pain right now.
Low back pain is the number one reason for absenteeism at work.
The number of lumbar spine fusions have gone up 171%.
There is a low back pain epidemic and a low back pain management epidemic in the United States.
Luckily, in the majority of cases, it is a treatable condition if approached from a researched, conservative approach. This article will cover what low back pain not, why current treatment models fail, and finally, what it actually is.
What It Is Not, & Why Pain Models Fail
Our bodies typically exhibit pain in an attempt to warrant a change, but only viewing and treating the pain generator is linked with poor clinical outcomes.
A standard medical approach attempts to describe what's wrong with the body by describing what is wrong with their anatomy. In the realm of back pain, the standard model attributes pain and limitations to movement to degeneration/arthritis.
From the Journal of the American Medical Association's October 2019 edition, Dr. Ganguli, a doctor at Harvard Medical School, examines the practices of nearly 400 medical doctors and their use of diagnostic imaging to correlate diagnosis to the patient's condition. He reports:
31% of imaging produces no findings at all. 14.8% of imaging produces meaningful outcomes. 52% of imaging produces incidental findings that do not correlate to the patient's condition.
99.4% of physicians reported that incidental findings were over pursued. When treatment began for incidental findings, 68% of patients got worse, and 70% reported the testing as a waste of time.
Almost all respondents experienced incidental findings that did not lead to clinically meaningful outcomes and yet caused harm to patients.
Along the spine, most advanced imaging (MRI, CT) shows degenerative findings. It’s important to note that these findings don’t describe why you are experiencing pain. Research has routinely shown that people without symptoms can show large amount of degeneration. A prior diagnosis of arthritis or degenerative disc disease does not mean you are subject to a lifetime of pain.
For example: A Systematic Review of Spinal Degeneration in Asymptomatic Populations by the Journal of American Neuroradiology published in April of 2015:
3,110 patients without symptoms were given an MRI.
20-year-old individuals without any symptoms showed: 37% had disc degeneration; 30% had a disc bulge, and 19% had tears in their discs.
80-year-old individuals without any symptoms showed: 96% had disc degeneration; 84% had a disc bulge, and 29% had tears in their disc.
The study concludes that imaging-based degenerative features are a part of normal aging and unassociated with pain.
Our discs slowly degenerate over time, and this can be a painless process. However, if abnormal forces wear our tissues down at an accelerated rate, the rapid breakdown of our discs induces inflammation, which can amplify a pain response.
A thorough doctor should look at degeneration for what it is. Our bodies degenerate and build bone spurs in an attempt to stabilize an area. More specifically, the joints that degenerate rapidly are the joints that move excessively in the wrong directions. Therefore, a doctor should examine WHY the body degenerates, not just accepting degeneration as the cause for their pain intrinsically. This is frequently missed by pain-based chiropractors and medical doctors alike. Using a hammer on screws is an ineffective treatment solution.
As an example:
An individual presents to his family medical doctor.
His medical doctor prescribes him an anti-inflammatory, muscle relaxant, or pain killing medication. Upon completion of his medication, the pain returns. After a few rounds of unsuccessful long term resolution, the medical doctor orders an MRI.
The MRI reveals degeneration, disc bulges, and arthritis (remember, this is equally found in people without any pain). These images are rarely correlated with a functional treatment.
A surgeon then operates on the spine.
A systematic review from Pain Journal November edition 2014 revealed:
Less than 20% of patients with low back pain received evidence-based information and advice from their family doctor.
25% of all patients presenting for low back pain to their family doctor were referred for imaging; 33% of all emergency room visits for low back pain were referred for imaging.
30% of patients with low back pain were given opioids from their family doctor; 60% of emergency room doctors prescribed opioids for low back pain.
"Large numbers of patients that saw a physician for low back pain received care that is inconsistent with evidence-based clinical practice guidelines. Usual care included overuse of imaging and opioid prescription, and underuse of advice and information."
From the November 2016 edition of the Journal of Pain Research, the division of pain medicine from John Hopkins University School of Medicine reports:
The number of lumbar spine fusions have gone up 171%.
The success rate for lumbar spine surgery is 35%.
65% of patients report no improvement, and 29.2% of patients report worsening symptoms following surgery.
It is estimated that 40% of all individuals who undergo lumbar spine surgery will have it repeated.
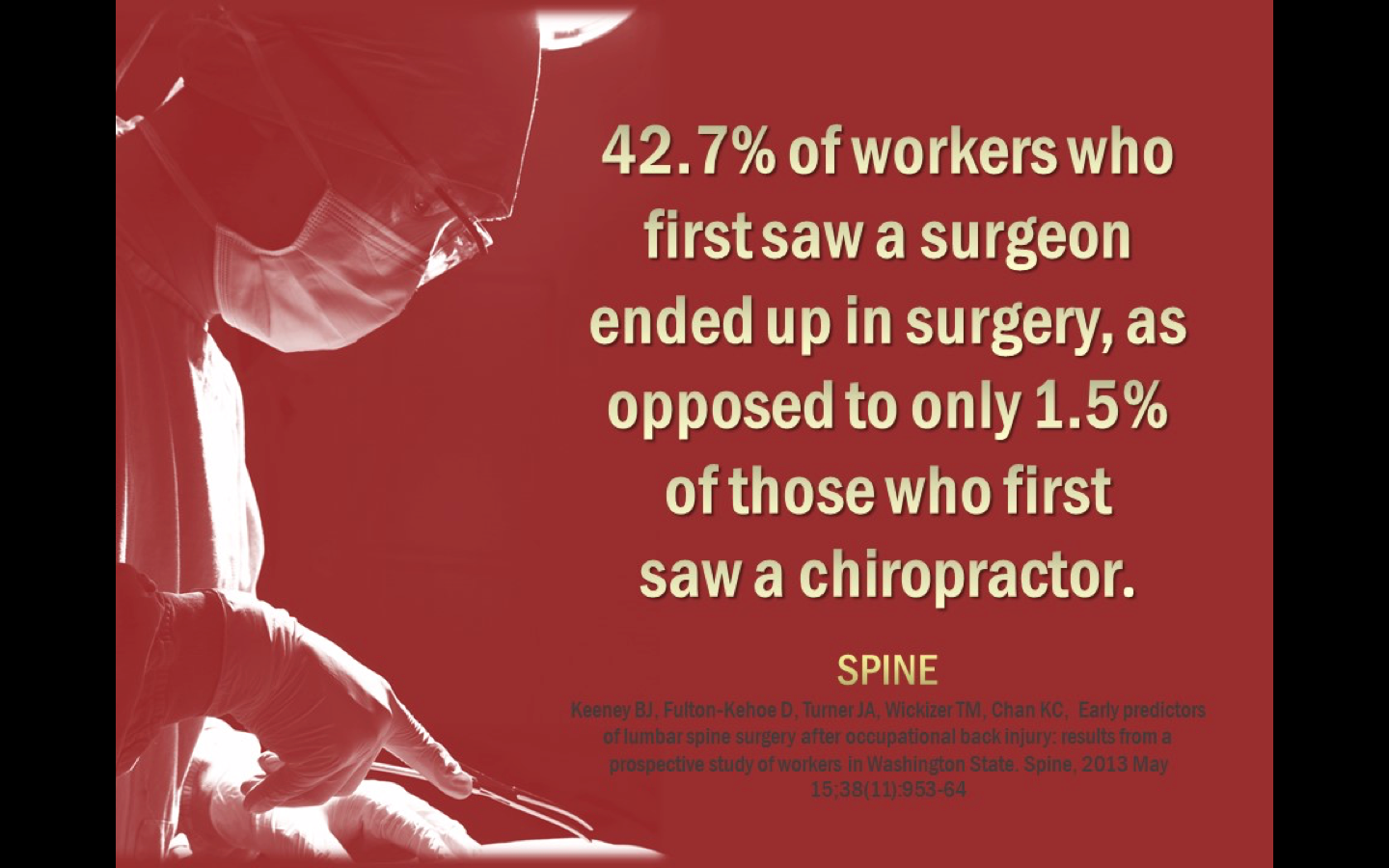
In a study from BMC Health services comparing chiropractic vs standard medical model (Not counting surgical costs):
In private healthcare plans: 92% of studies demonstrated that health care costs for low back pain were cheaper with chiropractic care compared to outpatient care from a medical doctor. The difference in health care costs who received chiropractic was, on average, 59%-70% cheaper.
In worker's compensation plans: 83% of studies demonstrated that health care costs for low back pain were cheaper with chiropractic care compared to outpatient care from a medical doctor. The difference in health care costs who received chiropractic was, on average, 91%-229% cheaper.
The findings suggested that usual care from a family medical doctor was rarely evidence-based, with many patients receiving bed rest, opioids, and physical modalities. After 6 months, patients who received chiropractic care was more likely to improve than those receiving usual care.
Describing degeneration (overloaded tissue) as the pain generator is not backed by evidence. It is a description that fails to identify why the body is degenerating rapidly. It's equivalent to constantly replacing the tread on your 3 tires that are wearing while ignoring the flat tire on the rear passenger side of your vehicle. Only by recognizing what low back pain is can we reach a solution.
What It Is
Low back pain tends to be mechanical in nature, as it frequently comes from the spine, discs, or surrounding soft tissues. It can be determined to be mechanical if it is affected by position or movement. This is because when we move, force is transferred onto various structures. The source for mechanical low back pain is found by examining which tissue is being overloaded. If a mechanical force caused the problem, then logic would have it that mechanical force can cause the solution. However, a doctor must examine why the tissue is being overloaded.
As an example In the Journal of Physical Therapy in Sports (2008):
48 people were examined and split into two groups of 24. One group of 24 reported significant low back pain, another group reported none. Researchers examined for any key distinctions between the groups.
The group that reported low back pain had significantly reduced total hip rotation and large differences between the movement of the right and left hip.
The group that did not have any low back pain had no differences in right and left total hip rotation.
These findings suggest that altered directional movement demands from hips that don't move properly will transfer extra movement to the spine, overloading the spinal structures. In this scenario, the spinal facet joint becomes the symptom generator, but the hip's inability to move becomes the mechanical dysfunction. Often, the true dysfunction is painless, and it can affect not only our mechanics, but it can also impact our nerves (subluxation) which control the functioning of our bodies.
Sadly, many chiropractors will zero in and adjust where the pain is, which provides relief for a short while, but re-presents after an extended period of time. Many chiropractors fail to find the true mechanical dysfunction because they only set their sights on pain generating structures.
Typically, mechanical dysfunction is found with joint restriction, muscular tightness from over-active muscles, and muscular weakness from under-active muscles. A restricted joint will not allow the joint to move, which alters our body's ability to properly utilize the musculature. Further, our joints need proper movement to nourish themselves. A lack of movement leads to inflammation, which amplify the pain signal.
A thorough chiropractor will free the joint, calm down the tight muscle, strengthen the weak muscle, and examine diet for inflammation control. By equipping the patient to train their weak muscles at home and work, the chiropractic visits just become check ins to make sure the joint is no longer restricted.
In the above scenario, if the patient exhibited left and right differences in hip mobility, the chiropractor may take an x-ray to determine structural causes that could affect treatment. By correlating the patient's structural anatomy AND their functional presentation, the chiropractor is equipped to identify the cause of the dysfunction driving their overloaded tissue (symptom generator).
In rare cases, back pain can be non-mechanical. Although rare, chiropractors are trained to assess and recognize these cases, and make the appropriate referral. Because back pain can be so complex and multi-factorial, a thorough assessment is critical.
Conclusion
Zeroing in and focusing on just the overloaded tissue/pain generator has low evidence for long term solutions. Identifying degeneration (overloaded tissue) is not backed by evidence. By identifying pain as mechanical and finding dysfunctions that fuel the mechanical overload, both structural and functional, a chiropractor can best equip you with the care needed to not just live pain free, long term, but to get your life back, doing the things you love.
For more information about our practice, please visit our website!
Remember that you were made to have life and have it more abundantly; You were made to thrive.
Sources
Baber, Zafeer, and Michael A Erdek. “Failed Back Surgery Syndrome: Current Perspectives.” Journal of Pain Research, Dove Medical Press, 7 Nov. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5106227/.
Brinjikji, W, et al. “Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations.” AJNR. American Journal of Neuroradiology, U.S. National Library of Medicine, Apr. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4464797/.
Dagenais, Simon, et al. “A Systematic Review Comparing the Costs of Chiropractic Care to Other Interventions for Spine Pain in the United States.” BMC Health Services Research, BioMed Central, 19 Oct. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4615617/.
Ganguli I, Simpkin AL, Lupo C, et al. Cascades of Care After Incidental Findings in a US National Survey of Physicians. JAMA Netw Open. 2019;2(10):e1913325. https://doi.org/10.1001/jamanetworkopen.2019.13325
Kamper, Steven J, et al. “What Is Usual Care for Low Back Pain? A Systematic Review of Healthcare Provided to Patients with Low Back Pain in Family Practice and Emergency Departments.” Pain, U.S. National Library of Medicine, 14 Nov. 2019, www.ncbi.nlm.nih.gov/pubmed/31738226.
Keeney, Benjamin J, et al. “Early Predictors of Lumbar Spine Surgery after Occupational Back Injury: Results from a Prospective Study of Workers in Washington State.” Spine, U.S. National Library of Medicine, 15 May 2013, www.ncbi.nlm.nih.gov/pubmed/23238486.
Reiman, Michael P, and J W Matheson. “Restricted Hip Mobility: Clinical Suggestions for Self-Mobilization and Muscle Re-Education.” International Journal of Sports Physical Therapy, Sports Physical Therapy Section, Oct. 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC3811738/.
Van Dillen, Linda R, et al. “Hip Rotation Range of Motion in People with and without Low Back Pain Who Participate in Rotation-Related Sports.” Physical Therapy in Sport : Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, U.S. National Library of Medicine, May 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC2597839/.
Will, Joshua Scott, et al. “Mechanical Low Back Pain.” American Family Physician, 1 Oct. 2018, www.aafp.org/afp/2018/1001/p421.html.